Dubai: Britain has rolled out its COVID-19 inoculation drive, becoming the first Western country to use the Pfizer-BioNTech vaccine outside trials. A 90-year-old British grandmother, Margaret Keenan, who turns 91 next week, was the first to receive it.
“I feel so privileged to be the first person vaccinated against COVID-19,” said Keenan, a former jewellery shop worker who has two children and four grandchildren.
Frontline health and social care staff, care home workers and those over 80 will get the jab first. A second dose is required in 21 days.
Britain last week became the first country to approve the Pfizer-BioNTech vaccine, raising hopes of a breakthrough in the pandemic, which has killed more than 1.5 million worldwide.
Britain has been one of the worst-affected countries in the world, with more than 61,000 deaths in the outbreak from 1.6 million cases.
Does this mean that we can abandon our masks and live like we have defeated the coronavirus?
Not quite. There are many things we still do not know about the coronavirus. The fight has just begun, but there’s light at the end of the tunnel.
The 81-year-old had the injection at University Hospital Coventry on Tuesday, 32kms from Stratford-Upon-Avon, the birthplace of his namesake, England’s greatest dramatist and poet.
Shakespeare’s shot inspired Twitter users, who joked “The Taming of the Flu”, “The Two Gentlemen of Corona”. Some asked if Margaret Keenan was patient 1A, then was Shakespeare “Patient 2B or not 2B?”
How will the vaccine protect me?
The vaccine prevented COVID-19 illness seven days after the second injection – which is about a month after the first shot.
Clinical trials so far have not been designed to determine if an immunised person can still spread the coronavirus to someone else. Some vaccines, such as hepatitis A, do provide such protection – known as sterilising immunity – but others do not. COVID-19 vaccine makers focused trials on determining whether the drug stopped people from getting ill.
It will also be several more months before it becomes clear how long the vaccination will protect someone from coronavirus infection.
Till then it is better to stay safe and follow the safety protocols.
How many doses are needed for a person?
The Pfizer-BioNTech vaccine has been developed with new messenger RNA technology using a manufactured fragment of the coronavirus’ genetic code. The immunisation is given in two doses, three weeks apart, and has been shown in trials to protect up to 95% of recipients from contracting COVID-19.
Side effects in trial volunteers were mostly mild to moderate, and cleared up quickly. The most severe side effects occurred after the second dose: fatigue in 3.8% of volunteers and headache in 2%. Older adults reported fewer and milder adverse events.
Can we go back to normal life now?
Since there is no evidence that the immunisation prevents transmission of the virus – and no vaccine is 100% effective – scientists call for continued vigilance, including mask-wearing, hand-washing and social distancing. Also, vaccination campaigns are unlikely to reach most people until the middle of 2021.
Will there be enough doses to inoculate everyone?
More than 10 billion doses of COVID-19 vaccines have been pre-ordered, including most of the 2021 manufacturing capacity for the leading candidates, according to the journal Nature.
WHO, UNICEF and the vaccine alliance Gavi and partners are working together to help prepare countries to be ready to introduce the vaccine.
70
%
of the world’s population needs to be inoculated to break the chain of the coronavirus, according to WHO
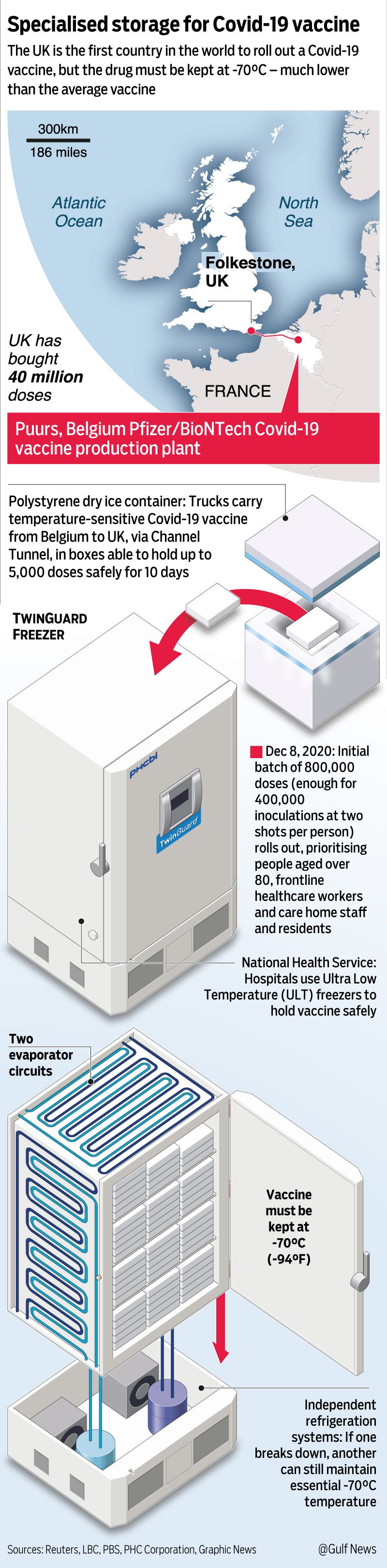
In the UK, about 800,000 doses are expected to be available within the first week. The roll-out is also a test case for Pfizer and BioNTech’s distribution networks. The vaccine must be stored at -70C (-94F) and only lasts five days in a regular fridge. While Britain is relatively small and has good infrastructure, the logistical challenges mean it will first be applied in 50 hospitals and cannot yet be taken into care homes.
The World Health Organisation estimates that 70 per cent of the world’s population needs to be inoculated in order to break the chain of the coronavirus. That works out to around 5.3 billion people.
In total Britain has ordered 40 million doses of the Pfizer/BioNTech vaccine. As each person requires two doses, that is enough to vaccinate 20 million people in the country of 67 million. The UK has ordered 357 million doses of seven different COVID-19 vaccines in all.
The US has ordered 100 million doses of the Pfizer vaccine.
What are the other vaccines in the pipeline?
More than 140 drugmakers and research groups around the globe have been racing to develop vaccines against COVID-19.
There are 87 preclinical vaccines in active development and 54 others in the three phases of trials. Six vaccines have already been approved for limited use in some countries.
A vaccine from Moderna was found to have a similar level of success in trials and is based on the same mRNA genetic technology that requires such ultra-cold storage.
Read more
- When do I get a COVID-19 vaccine?
- Global, UAE stock markets driven up by hopes of imminent vaccine
- COVID-19: Bahrain becomes second country in world to approve Pfizer vaccine
- MMR vaccine for children helps prevent severe COVID-19: Study
- Vaccine approved: UK authorisation for Pfizer/BioNTech mRNA vaccine marks revolution in medicine
The third vaccine to have had trial success, developed by AstraZeneca and Oxford University, is viewed as offering one of the best hopes for many developing countries because it is cheaper and can be transported at normal fridge temperatures.
Late-stage trials found it had an average success rate of 70%.
Till I get a vaccine, should I continue wiping down groceries?
Experts say it’s not necessary for most people.
The coronavirus spreads mainly through the respiratory droplets people spray when talking, coughing, sneezing or singing. It’s why health experts stress the importance of wearing masks and social distancing. Experts still recommend cleaning surfaces – especially frequently touched spots that infected people might have recently touched. That will also help reduce risk from other germs that haven’t gone away in the pandemic. People caring for those at risk for severe illness if infected might also want to take the precaution of wiping down any packages.

Image Credit: AFP
But experts say to keep things in perspective. The virus is fragile and doesn’t survive easily outside the body for long, they note. Earlier tests that found the virus on surfaces might just be detecting traces of the virus, not live virus capable of infecting people. Early studies that showed the pathogen could linger on surfaces for days were conducted under laboratory conditions” the virus likely couldn’t survive that long in real life.
Dr. John Brooks, chief medical officer for the COVID-19 response at the US Centers for Disease Control and Prevention, said people should do what makes them comfortable. But he said if people unpack groceries without touching their faces and then washing their hands afterward, “I think that may be sufficient.”
When was the first vaccine discovered?
The first vaccine was discovered more than 200 years ago, when English doctor Edward Jenner stimulated an immune response in a child.
Here’s a brief history of the vaccine.
1796: The first vaccine
Deadly and highly contagious smallpox, transmitted through open sores that scarred millions for life, ravaged populations for centuries until English doctor Edward Jenner notices that milkmaids who got cowpox never get smallpox.
In 1796 he inoculates a child with the harmless version of the disease to stimulate an immune response. Despite repeated exposure, the child never falls ill. Vaccination is born.
1853: Poxy policy
The smallpox vaccine becomes mandatory for all British children in 1853, but this provokes an immediate backlash. Many object for religious reasons or see the policy as infringing of individual liberties. A conscience clause is added to the law in 1898 to allow people to opt out.
1885: Pasteur and rabies
French scientist Louis Pasteur develops a rabies vaccine from a more benign strain of the disease. It appears successful when he gives it to a child bitten by a rabid dog. Vaccine sceptics however accuse Pasteur of trying to develop “laboratory rabies” to increase his profits.
1920s: TB, diphtheria, tetanus
A vaccine against typhoid is developed at the end of the 19th century, followed by several crucial shots in the 1920s: the 1921 Bacille Calmette-Guerin (BCG) vaccine against tuberculosis and shots against diphtheria in 1923, tetanus in 1926 and whooping cough in 1926.
It is also in the 1920s that aluminium-containing agents are first used in vaccines to increase their efficiency – an ingredient that will spark vaccine scepticism later on, especially in France.
1944: Flu vaccine
The first vaccine campaign against the seasonal flu targets US soldiers fighting in Europe in 1944-45, with a new shot developed each year.
In the 1950s, when polio vaccination was a US government priority, megastar Elvis Presley lent himself to the cause, getting the shot live on the primetime “Ed Sullivan Show”.
In the 1970s a campaign to innoculate Americans against a supposedly devastating strain of swine flu grounds to a halt, however, when the pandemic fails to materialise and some 450 of those vaccinated unnecessarily develop Guillain-Barre syndrome which can cause paralysis. The incident continues to fuel vaccine scepticism.
1980: Smallpox wiped out
The last natural case of smallpox is diagnosed in Somalia on October 26, 1977 and the World Health Organization (WHO) declares the illness officially eradicated in 1989 thanks to a global vaccination campaign.
A similar campaign to eradicate polio has been hugely successful, wiping it out in Africa. The disease lingers on in Pakistan and Afghanistan.
1998: Fake study, real damage
In 1998 a study published in the prestigious Lancet medical journal suggests a link between the MMR (measles, mumps and rubella) vaccine and autism.
The main plank of it, however, had been falsified by its author Andrew Wakefield who was later barred from the profession. Yet the debunked study is still cited by “anti-vaxers”.
2009: H1N1 debacle
In 2009 an H1N1 – or swine flu – outbreak sets off alarm bells around the world. Although related to the infamous 1918 flu strain, the virus turns out to be far less consequential, killing 18,500 people. The waste from millions of unused vaccines prompts criticism of the WHO’s handling of the outbreak.
In addition, Sweden, where more than 60 per cent of the population were vaccinated, was traumatised when hundreds of people who got the jab were later diagnosed with narcolepsy – a chronic sleep disorder characterised by overwhelming daytime drowsiness and sudden attacks of sleep.
– with inputs from agencies


